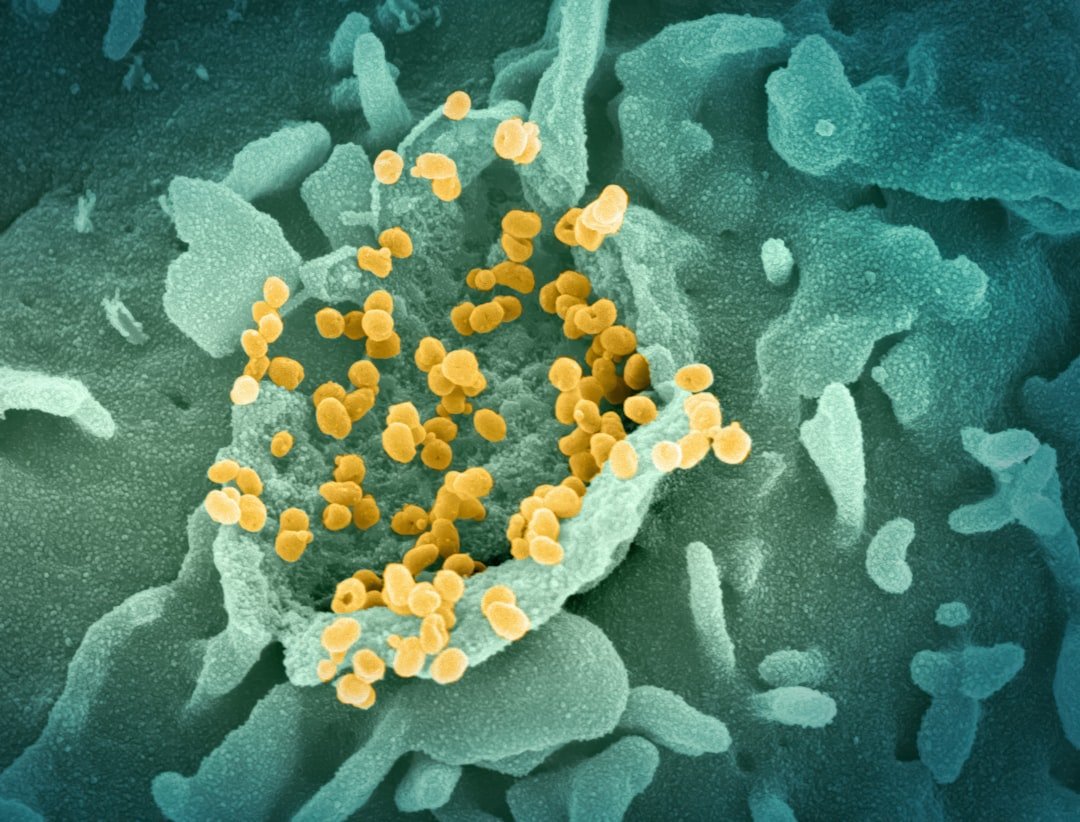
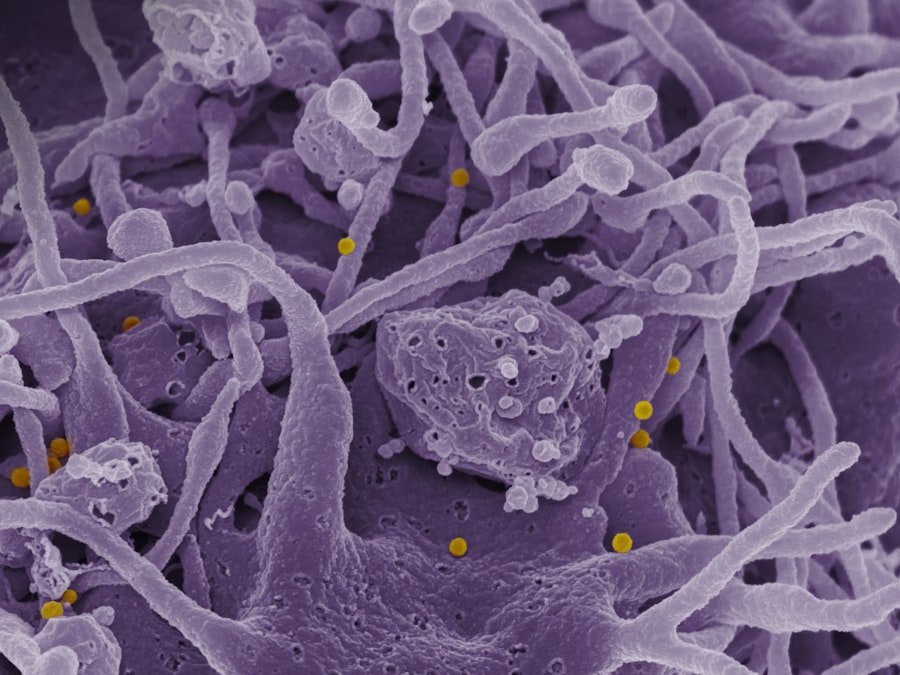
Antimicrobial resistance (AMR) is a phenomenon where microorganisms such as bacteria, viruses, fungi, and parasites evolve to resist the effects of medications that once effectively treated them. This resistance can occur through various mechanisms, including genetic mutations and the acquisition of resistance genes from other organisms. The World Health Organization (WHO) has identified AMR as one of the most significant threats to global health, as it complicates the treatment of infectious diseases, leading to prolonged illness, increased healthcare costs, and a higher risk of mortality.
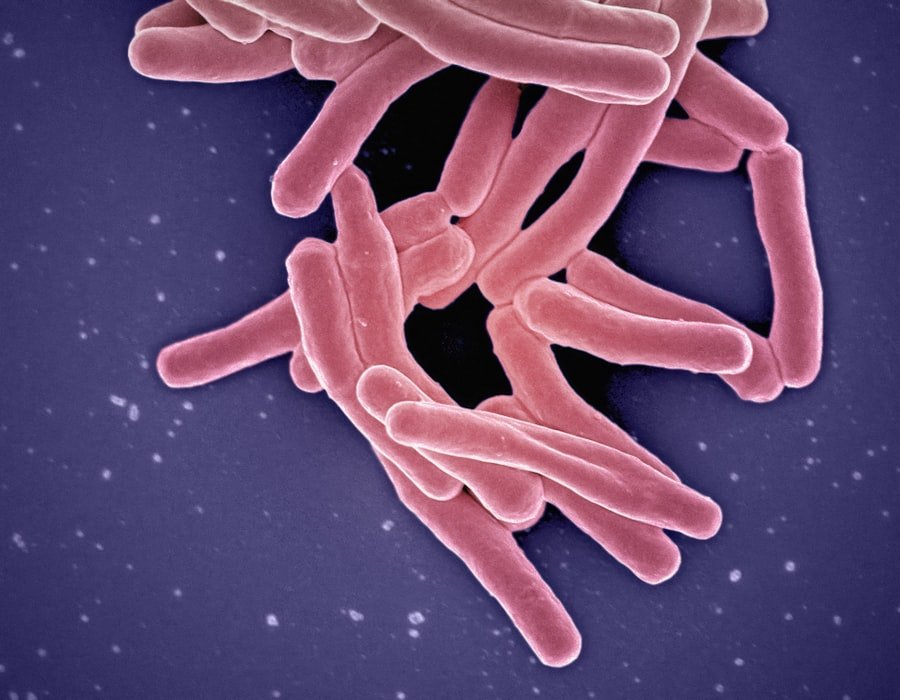
The emergence of resistant strains has been documented across a wide range of pathogens, including Escherichia coli, Staphylococcus aureus, and Mycobacterium tuberculosis, which have all shown alarming levels of resistance to commonly used antibiotics. The understanding of AMR is further complicated by its multifaceted nature. It is not merely a clinical issue but also a public health challenge that intersects with environmental and agricultural practices.
For instance, the use of antibiotics in livestock farming has been linked to the development of resistant bacteria that can be transmitted to humans through the food chain. Additionally, inadequate sanitation and hygiene practices can facilitate the spread of resistant pathogens in communities. As such, AMR is not confined to healthcare settings; it permeates various sectors, necessitating a comprehensive approach to tackle its implications effectively.
Key Takeaways
- Antimicrobial resistance is the ability of microorganisms to resist the effects of antimicrobial drugs, leading to ineffective treatment of infections.
- Antimicrobial resistance has a significant impact on global public health, leading to increased mortality, prolonged illness, and higher healthcare costs.
- Factors contributing to antimicrobial resistance include overuse and misuse of antibiotics, poor infection prevention and control, and lack of access to clean water and sanitation.
- Overuse and misuse of antibiotics, including unnecessary prescriptions and improper use in agriculture, contribute to the development of antimicrobial resistance.
- Antimicrobial resistance has economic and social consequences, including increased healthcare costs, loss of productivity, and reduced effectiveness of medical treatments.
The Impact on Global Public Health
The impact of antimicrobial resistance on global public health is profound and far-reaching. Infections caused by resistant organisms lead to longer hospital stays, the need for more expensive medications, and an increased risk of death. According to estimates from the Centers for Disease Control and Prevention (CDC), at least 2.8 million people in the United States are infected with antibiotic-resistant bacteria each year, resulting in over 35,000 deaths.
This situation is mirrored globally, with the WHO estimating that AMR could cause 10 million deaths annually by 2050 if left unchecked. The burden of AMR disproportionately affects vulnerable populations, including children, the elderly, and those with compromised immune systems. Moreover, AMR poses significant challenges to modern medicine.
Surgical procedures, cancer treatments, and organ transplants rely heavily on effective antibiotics to prevent and treat infections. The rise of resistant infections threatens the success of these interventions, leading to increased morbidity and mortality rates. The economic implications are equally concerning; healthcare systems face escalating costs due to longer hospitalizations and the need for more complex treatments.
The overall impact on public health systems can lead to a vicious cycle where resources are strained, further hindering efforts to combat infectious diseases.
Factors Contributing to Antimicrobial Resistance
Several factors contribute to the rise of antimicrobial resistance, creating a complex web of challenges that must be addressed. One primary factor is the over-prescription and inappropriate use of antibiotics in human medicine. In many cases, antibiotics are prescribed for viral infections where they are ineffective, or patients do not complete their prescribed courses, allowing surviving bacteria to develop resistance.
This misuse is often exacerbated by a lack of awareness among both healthcare providers and patients regarding the appropriate use of these medications. In addition to human medicine, agricultural practices play a significant role in the development of AMR. The routine use of antibiotics in livestock for growth promotion and disease prevention has been linked to the emergence of resistant strains that can be transmitted to humans through food consumption or direct contact with animals.
Furthermore, inadequate infection prevention and control measures in healthcare settings contribute to the spread of resistant pathogens. Poor sanitation and hygiene practices in both community and healthcare environments facilitate the transmission of these organisms, highlighting the need for comprehensive strategies that address all contributing factors.
The Role of Overuse and Misuse of Antibiotics
| Topic | Metrics |
|---|---|
| Overuse of Antibiotics | Percentage of antibiotics prescribed unnecessarily |
| Misuse of Antibiotics | Number of antibiotic prescriptions for viral infections |
| Antibiotic Resistance | Rate of antibiotic-resistant infections |
| Public Awareness | Percentage of people aware of the dangers of overuse and misuse of antibiotics |
The overuse and misuse of antibiotics are critical drivers of antimicrobial resistance. In many healthcare systems worldwide, antibiotics are prescribed without sufficient diagnostic testing or clinical justification. This practice not only fails to address the underlying cause of illness but also contributes to the selection pressure that fosters resistance.
For instance, studies have shown that countries with high rates of antibiotic consumption often report higher levels of resistance among common pathogens. This correlation underscores the urgent need for stewardship programs aimed at optimizing antibiotic use in clinical settings. In addition to human medicine, the agricultural sector’s reliance on antibiotics exacerbates the problem.
Livestock producers often administer antibiotics not only for treating infections but also for promoting growth and preventing disease in healthy animals. This practice leads to the proliferation of resistant bacteria in animal populations, which can subsequently enter the human population through food products or environmental pathways. The interconnectedness between human health and animal agriculture necessitates a One Health approach that recognizes the shared risks associated with antibiotic use across different domains.
The Economic and Social Consequences of Antimicrobial Resistance
The economic consequences of antimicrobial resistance are staggering and multifaceted. Healthcare systems face increased costs due to longer hospital stays, more intensive care requirements, and the need for more expensive alternative treatments when first-line antibiotics fail. A study published in “Health Affairs” estimated that AMR could cost the U.S.
economy up to $20 billion annually in direct healthcare costs alone, not including lost productivity due to illness or premature death. These financial burdens extend beyond individual patients; they strain public health resources and can lead to increased insurance premiums and out-of-pocket expenses for families. Socially, AMR exacerbates health inequities both within and between countries.
Vulnerable populations—such as those living in low-income settings or without access to quality healthcare—are disproportionately affected by resistant infections due to limited treatment options and inadequate healthcare infrastructure. This disparity can lead to a cycle of poverty and ill health that is difficult to break. Furthermore, as resistant infections become more prevalent, public trust in healthcare systems may erode, leading individuals to seek alternative treatments or avoid seeking care altogether.
Strategies for Addressing Antimicrobial Resistance
Addressing antimicrobial resistance requires a multifaceted approach that encompasses various strategies across different sectors. One critical component is the implementation of antibiotic stewardship programs in healthcare settings aimed at optimizing prescribing practices. These programs involve educating healthcare providers about appropriate antibiotic use, promoting adherence to clinical guidelines, and implementing monitoring systems to track antibiotic prescriptions and resistance patterns.
In addition to stewardship programs, enhancing infection prevention and control measures is essential in both healthcare facilities and community settings. This includes promoting hand hygiene practices, ensuring proper sterilization techniques in medical procedures, and improving sanitation infrastructure in communities. Vaccination programs also play a vital role in reducing the incidence of infections that require antibiotic treatment, thereby decreasing the selective pressure that drives resistance.
Furthermore, there is a pressing need for research and development into new antibiotics and alternative therapies. The pharmaceutical industry faces significant challenges in developing new antimicrobials due to high costs and regulatory hurdles; thus, innovative funding models and incentives are necessary to stimulate research in this area. Public-private partnerships can facilitate collaboration between governments, academia, and industry to accelerate the discovery of novel treatments.
The Need for Global Cooperation and Action
The global nature of antimicrobial resistance necessitates international cooperation and coordinated action among countries. AMR knows no borders; resistant pathogens can easily spread across regions through travel, trade, and environmental pathways. Therefore, global surveillance systems are essential for monitoring resistance patterns and sharing data among nations.
Initiatives such as the Global Antimicrobial Resistance Surveillance System (GLASS) established by WHO aim to standardize data collection and reporting on AMR globally. Moreover, international agreements and frameworks can help guide national policies on antibiotic use in both human health and agriculture. The World Health Assembly has adopted resolutions urging member states to develop national action plans addressing AMR tailored to their specific contexts.
These plans should encompass strategies for improving antibiotic stewardship, enhancing infection prevention measures, promoting research into new treatments, and fostering public awareness campaigns about responsible antibiotic use.
The Future of Antimicrobial Resistance and Public Health
Looking ahead, the future landscape of antimicrobial resistance presents both challenges and opportunities for public health. As resistant infections continue to rise globally, there is an urgent need for sustained commitment from governments, healthcare providers, researchers, and communities alike. The integration of AMR considerations into broader health policies will be crucial for mitigating its impact on public health systems.
Advancements in technology may offer new avenues for combating AMR as well. Innovations such as rapid diagnostic tests can help ensure appropriate antibiotic prescribing by enabling clinicians to identify infections more accurately and quickly. Additionally, research into bacteriophage therapy—using viruses that infect bacteria—holds promise as an alternative treatment strategy against resistant infections.
Ultimately, addressing antimicrobial resistance will require a paradigm shift in how society views antibiotics—not merely as a quick fix but as precious resources that must be preserved through responsible use and stewardship. By fostering a culture of accountability around antibiotic prescribing practices and investing in research and education initiatives, we can work towards a future where effective treatments remain available for generations to come.
FAQs
What is antimicrobial resistance (AMR)?
Antimicrobial resistance (AMR) occurs when microorganisms such as bacteria, viruses, fungi, and parasites evolve and become resistant to the drugs used to treat the infections they cause.
Why is antimicrobial resistance a global public health emergency?
Antimicrobial resistance is a global public health emergency because it threatens the effective prevention and treatment of an ever-increasing range of infections caused by bacteria, parasites, viruses, and fungi. This can lead to prolonged illness, disability, and death.
How does antimicrobial resistance occur?
Antimicrobial resistance occurs naturally over time, usually through genetic changes. However, the misuse and overuse of antimicrobial drugs accelerate this process.
What are the causes of antimicrobial resistance?
The main causes of antimicrobial resistance include the overuse and misuse of antimicrobial drugs in humans, animals, and agriculture, as well as poor infection prevention and control practices.
What are the consequences of antimicrobial resistance?
The consequences of antimicrobial resistance include increased morbidity and mortality, prolonged illness, higher medical costs, and the potential for the spread of infectious diseases.
How can antimicrobial resistance be addressed?
Addressing antimicrobial resistance requires a coordinated and multifaceted approach, including improving infection prevention and control, promoting the appropriate use of antimicrobial drugs, investing in research and development of new antimicrobial drugs, and strengthening surveillance and monitoring of antimicrobial resistance.